I am sharing this here as I feel it is important to talk about these things and honestly the sudden change in my HRT and drop to low levels has been pretty catastrophic for me as it often can for for people in surgical menopause. Hopefully I can get hold of my specilaist and get back to my normal self over Xmas. I will be dropping the letter into my doctor surgery later today.
Dear XXX Doctors,
I am a patient at XXX and wanted to raise an issue I ran into recently regarding ERT. I am a 50 year old woman and have been in surgical menopause since 2019. I did not initially fare terribly well on ERT and as a result sought the advice of a recognised menopause specialist registered with the BMS who as well as working privately runs NHS clinics. I initially consulted with her on the continuation of night sweats in October of 2021. She suspected I was not absorbing the transdermal oestradiol terribly well and recommended I increase estradot patches to 150 mcg. After this my night sweats, lethargy and hot flushes resolved.
Since that point aside from the odd infection I have remained generally in good health, my blood pressure is fine, cholesterol and all other blood markers appear to be within healthy parameters. I continued running my business and working on part time law PhD. All was in general fine.
On October the 23rd of this year Dr GP contacted me out of the blue. He felt I was on too high an ERT dose and wanted to drop my dosage. Which he did switching me from the 150 mcg patches to 4 pumps of estrogel. He believed that I would actually feel fine on that dosage and should I not after 6 weeks or so he would arrange blood tests to see if was absorbing the gel. At the recommendation of Dr Specialist when I began to have serious issues sleeping I increased to 5 pumps a day. Over the past 2 months since the change in my ERT I have had quite serious night time hot flushes that result in disturbed sleep, extremely low energy, I have struggled to concentrate and had to take time out of my PhD and felt so tired and actually at times very unwell I had to take time of work. I went from exercising 6 days a week and walking around 13000 to 15000 steps a day to struggling to exercise 3 to 4 times a week and walking 8000 steps a day. I also gained a few pounds in the process. However, I persevered believing that the doctor had my best interests at heart.
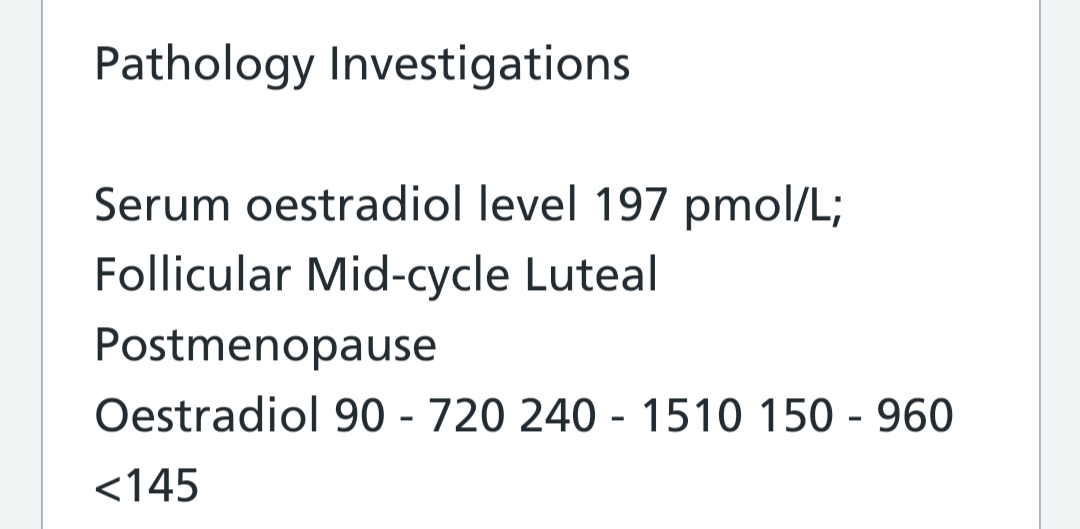
My oestradiol level was checked on the 13th of December and came back at 197 pmol/l (a low level) I also appear to have a higher than normal SHBG which may further be inhibiting absorption. Overall it is clear that I am not absorbing the transdermal gel terribly well. This is the case for some individuals. Dr Louise Newson has previously covered the reasons for this which may include the difference in skin thickness or distribution of capillaries[1]. It is important to note that the amount of medication applied is not the same as the amount of medication absorbed and some individuals are quite simply poor absorbers[2]. When my blood test results returned at the low end of normal and as I was suffering the return of symptoms my assumption was that it would be acknowledged that I was a poor absorber and would be returned to a dosage that allowed me to be free of symptoms and lead a decent quality of life. To my surprise Dr GP stated that he could not support a prescription for above the standard highest dose even with the evidence he requested provided. He suggested that I unofficially use more than the official prescription, but this leaves me with a situation where I may run out early. I also do not understand the logic.
I questioned why this was his recommendation and he stated that there was no evidence as to the safety associated with higher doses, however if I am not absorbing the majority of the gel I fail to understand how I am receiving a higher dose. Dr GP also stated that it was due to NICE guidelines. I could not find a statement in the NICE menopause section prohibiting higher doses in order to control symptoms, in fact the general guidance appears to be to adjust dosage according to response the guidelines also state “Adopt an individualised approach at all stages of diagnosis, investigation and management of perimenopause and menopause”[3] he also cited the main concern as being the risk of breast cancer however the NICE guidelines state “HRT with oestrogen alone is associated with little or no change in the risk of breast cancer”[4] The American Cancer Association states “estrogen-only HRT is not linked to a higher risk of breast cancer. The Women’s Health Initiative studies also found no increase in breast cancer risk in women using systemic oestrogen-only HRT.”[5] Even in women with the BRCA1 mutation who have undergone hysterectomies oestrogen only replacement does not appear to have any increased risk of breast cancer[6].
The other risks associated with ERT such as blood clots are commonly accepted to not be a risk with transdermal methods. I am not sure what risks I am avoiding then by having my oestradiol levels kept at a level that is no longer controlling menopausal symptoms. In fact there is research that indicates in the 50 to 60 age group women who have had hysterectomies and oophorectomies who avoid ERT are at an overall higher risk of all cause mortality[7]
When I raised the potential benefits of ERT to bone density which needs according to research to have blood levels of above 250 pmol/l in order to be effective I was informed that ERT was not given for that nor was it seen as relevant, the control of symptoms was the only reason for prescribing. An interesting statement when a patient raises it as a concern in particular when it is considered that falls are most common cause of injury related deaths in over 75 year olds and injury in over 65 year old. The issue being breaks which of course is far more likely with low bone density[8].
All in all I have been placed in a situation where I went from feeling well and active to not sleeping, gaining weight, feeling very unwell and unable to work plus not wanting to exercise. I was then told that fundamentally this was for my benefit. The appointment itself was classified as “women’s health”. I would be very interested to have it explained to me how gaining weight, losing work, not being able to pursue my PhD, not sleeping and becoming more inactive is going to benefit my health long term when all research would indicate otherwise. I suspect that the answer would be that I must just carry on as normal regardless of how awful I feel, women have historically often been told we must just put up with a lower quality of life and expect less, I did hope that in 2023 we were moving beyond that.
Then there is the matter of how this was undertaken which I feel was somewhat disingenuous, had at the outset the doctor explained that regardless of the outcome of drop in dosage, regardless of any return of symptoms and regardless of any blood results confirming poor absorption he would simply not prescribe above the standard dosages it would have been rather more honest. At which point I would have sought advice from the menopause specialist, not reduced or changed my ERT and asked to undertake blood tests to ascertain my levels at that point. I suspect in doing so I would have avoided a few rather unpleasant months. I presume that the real reason has little to do with my health or wellbeing which has done nothing but deteriorate since Dr GP decided to call me in October and more to do with cost reduction.
I am going to see the menopause specialist with my blood results as soon as I can, which may be tricky over Christmas. I am lucky that I can afford to do so but many other women would not be able to do so and they deserve a quality of life. Being over 50 or in menopause surgical or otherwise does not mean our day to day ability to function in the world should be viewed as so utterly meaningless and insignificant. We still have a great deal to contribute and for those who menopause symptoms are significant HRT or ERT may be a part of being able to do so. However that means ERT/HRT at a level that actually controls symptoms. It may well be necessary to check that levels are within normal ranges via blood tests, if the blood tests come back at the lower end of the range and symptoms are present the logical approach would be to adjust the dosage not tell the patient that they should be fine regardless of whether they are. Women deserve better.
Kind regards
Samantha Kelly
[1] https://www.balance-menopause.com/menopause-library/hrt-doses-explained/
[2] Armston A, Wood P. Hormone replacement therapy (oestradiol-only preparations): can
the laboratory recommend a concentration of plasma oestradiol to protect against
osteoporosis? Ann Clin Biochem. 2002;39(Pt 3):184-93.
[3] https://www.nice.org.uk/guidance/ng23/chapter/Recommendations#individualised-care
[4] https://www.nice.org.uk/guidance/ng23/chapter/Recommendations#long-term-benefits-and-risks-of-hormone-replacement-therapy
[5] https://www.breastcancer.org/risk/risk-factors/using-hormone-replacement-therapy
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6143051/
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3780684/
[8] https://www.ageuk.org.uk/latest-press/articles/2019/may/falls-in-later-life-a-huge-concern-for-older-people/